The necessity of testing during the COVID-19 pandemic
As the number of confirmed cases of COVID-19 increases, our ability to quickly test and identify patients with COVID-19 is critically important. Without knowing who has the virus, we are unable to isolate those who are infected and have turned to social distancing as our only means to slow the spread.
This level of uncertainty has had a profound impact on the way we conduct our daily lives, forcing us to assume everyone around us is infected. Beyond that, this uncertainty limits our ability to forecast what is to come. Public health professionals must rely heavily on assumptions and data generated by other countries that have come through on the other side of curve to infer rates of transmission, hospitalization and death caused by the disease. As the situation evolves, the development and broad deployment of testing specific to COVID-19 will enlighten us, and dramatically improve our ability to track infections of both individuals and populations.
Current testing availability and limitations
For testing to be effective, we need both rapid, accurate tests and laboratories that are qualified to run them. At the start of the outbreak in the U.S., all COVID-19 testing was conducted in CDC laboratories, which dramatically limited the capacity for testing and created a backlog that increased wait time for results. As the number of cases of suspected COVID-19 continued to climb, the CDC extended testing capability to U.S. public health laboratories to increase regional availability and capacity. The CDC is now also allowing testing through clinical and commercial laboratories certified under the Clinical Laboratory Improvement Amendments (CLIA) to perform high-complexity tests, dramatically expanding the resource pool for execution of testing, and enhancing the speed at which samples can be transported to and run at testing facilities.
The number and type of test kits available is also expanding daily, as the FDA works with test kit manufacturers to review applications for in vitro diagnostic (IVD) emergency use authorization. Thirty-two IVD test kits have been granted authorization for use during the crisis as of April 8, 2020. There are still many challenges in procuring and producing reagents and test kits, deploying them across the country and pairing them with the appropriate labware, reagents, and specialized equipment required to execute the tests and analyze the results, but we are moving in the right direction.
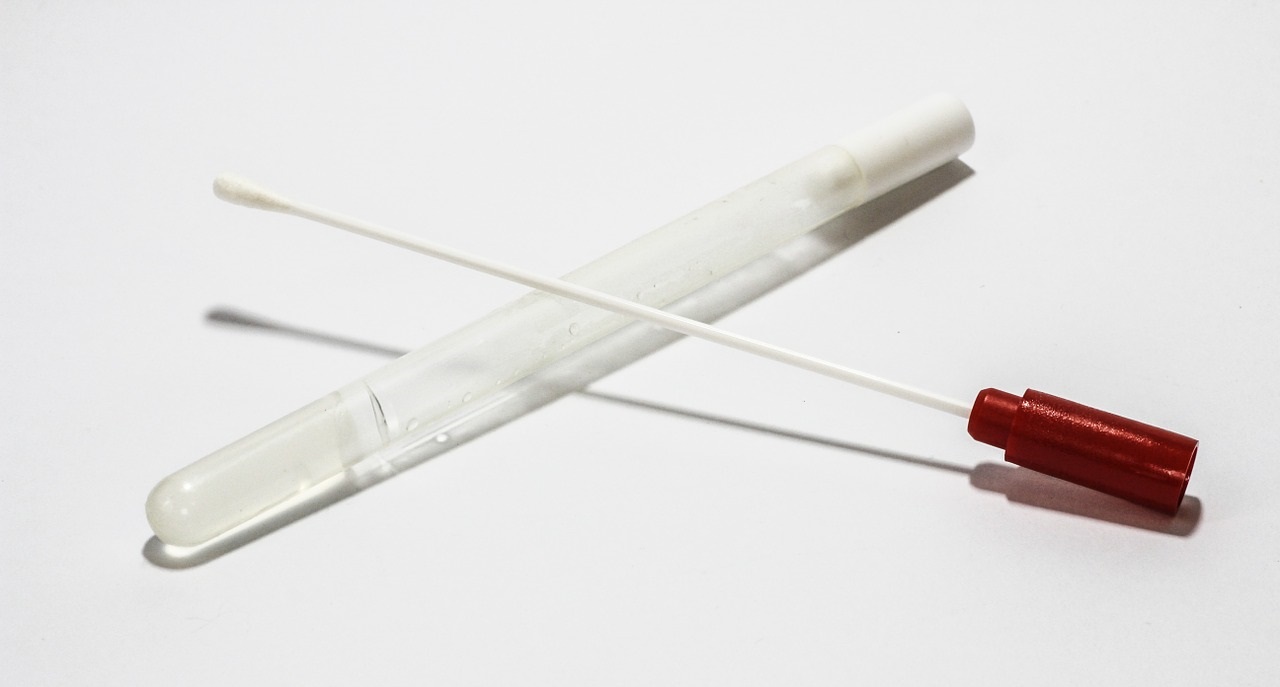
The early focus of diagnostic testing has been identifying those with active infections who could spread the virus to others. This testing works by isolating, amplifying and detecting the presence of COVID-19 viral genetic material, typically RNA, in respiratory samples collected from patients with suspected infection. This testing can identify a person with a detectable viral load of COVID-19, regardless of whether they are experiencing symptoms. If deployed strategically, testing could identify those in the population that are currently asymptomatic carriers of the virus, giving greater insight into the true breadth of infection and providing a path to reduce spread from these carriers through quarantine.
At present, the limited availability of COVID-19 tests has prompted the CDC to provide guidelines for testing that classify patients into three levels of priority. First priority is given to patients that have been hospitalized and health care workers that are symptomatic. The second priority level is reserved for symptomatic first responders and patients over 65 years of age, with underlying health conditions and those in long-term care facilities who are also showing symptoms of the virus. A third level of priority includes symptomatic individuals, as well as health care workers and first responders that are not displaying symptoms, and individuals with mild symptoms in communities with high COVID-19 hospitalization rates. There is currently no priority given to testing individuals without symptoms who may be carriers for the disease. Likewise, there are insufficient resources both to conduct aggressive contact tracing, where those who have had contact with someone who is positive for the virus, and testing of those contacts. This strategy, while appropriate given limitations in testing, results in a significant number of infected individuals going undetected. As the supply of tests rises to meet demands, these practices will evolve and bring about greater capability for detection of the disease.
Next-steps in diagnostic evaluation of COVID-19
As our response to COVID-19 evolves, diagnostic tests will need to serve an additional function to identify those that have developed an immune response to the virus. This type of testing detects the presence of antibodies to the virus generated through progression of the body’s natural response to infection. It can also provide a means to examine the true prevalence of the virus by identifying the portion of the population who experienced active infection in the past. This information can serve to improve our understanding of the virus and improve our modeling of the progression of the disease through the population. This type of testing will also be used to detect immunity acquired in response to a vaccine to determine the effectiveness of vaccines for COVID-19 in current clinical trials.
As our ability to make, distribute and run COVID-19 tests accelerates, so will our understanding. Only then can we make informed decisions of how to best carry on through this pandemic. The collective hope is that social distancing is decreasing the rate of transmission, and that the U.S. will soon experience a decline in new cases of COVID-19 like that observed in China and Italy. However, until an effective vaccine is made available, we must remain vigilant. The risk of subsequent waves of infection will remain, and super-spreader events, where one undetected individual with COVID-19 infects large numbers of others, could be catastrophic.
As people return to work and school, and as travel resumes, the ability to effectively test for and identify pockets of the disease will become even more important for the protection of public health. We will need to act quickly to enact regional social distancing practices anytime rates of confirmed cases rise to avoid overwhelming local health care systems and prevent broader spread of the virus. The need for these mitigation strategies is already on display in other parts of the world, including parts of China, Singapore and Taiwan, where a resurgence of cases occurred after restrictions eased.
Testing will remain a pivotal tool to assess and ultimately control the spread of COVID-19 as we aim to return to a more normal, albeit monitored, way of life. Over the near-term, wide-spread availability and use of testing should be both our focus and our best defense.
Author: Sarah Marking
Sarah Marking is a Senior Quality Scientist who recently joined Venebio Group, LLC. She earned her MS in biology from University of Maryland Baltimore County where she researched the neurobiology of chemical sensory systems before beginning her career in diagnostics. She brings her experience in translational medicine, operational quality, and management of large, interdisciplinary teams to Venebio, partnering with clients to help reach their strategic goals.
